BETTER BODY BALANCE
Introduction to Muscular Dystrophy: Raising Awareness for Future Practitioners
Author: Jordan Mathie
Introduction to MD
This post aims to raise awareness about a specific type of genetic neurological condition,
Muscular Dystrophy (MD). In this post I will highlight what MD is and how it affects the body,
how it impacts daily life and what we can learn from those who live with MD.
During my time as a student of Kinesiology, I have spent much of my hands on learning
with patients that are challenged with neurological conditions. I had never heard of MD before
and learned about it during my time in a practicum. During this time, gratefully, I was introduced
to Jane, a long time patient of my preceptor who is overcoming the daily challenges of life from
MD. Jane was very kind to let me interview her about some of the hardships, practical details,
and experiences she has experienced with MD. I will be referencing Jane throughout this post as
a source.
What is Muscular Dystrophy?
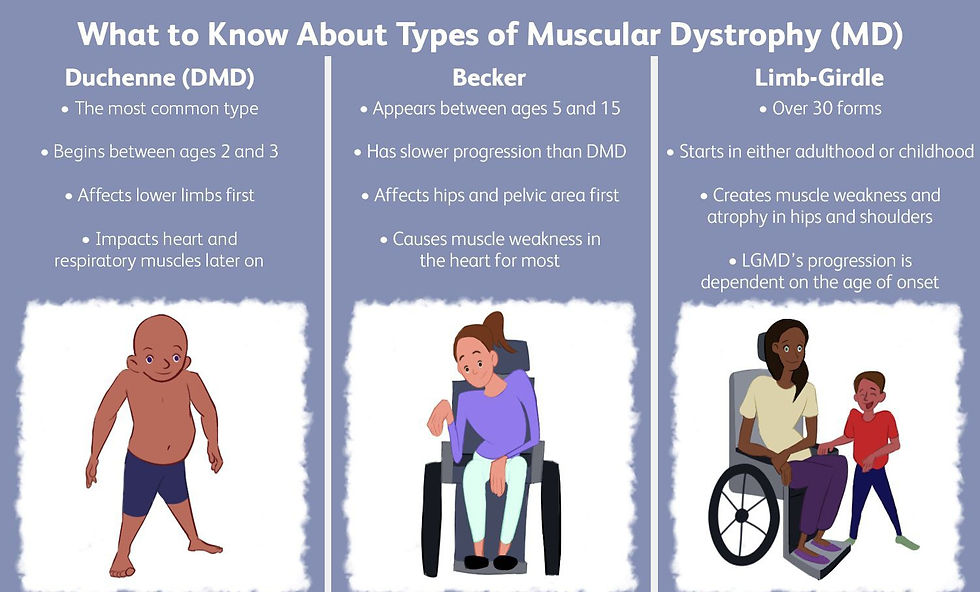
There are many types of MD, over 30, which can have effects on a multitude of
physiological systems like the heart, glands eyes, gastrointestinal system and more. According to
the National Institute of Neurological Disorders and Stroke (NINDS), MD is found to damage
the integrity of the muscle fiber. Looking closer at the muscle fiber, Dystrophyn, a protein
complex membrane that protects damage to a contracting muscle, is not functioning. This causes
excess calcium build up in the muscle fiber eventually causing them to die. Dead muscle fibers
are unable to receive an action potential, which is a signal telling the muscle to fire or contract
from the brain. This would eventually lead to the atrophy of the whole muscle group or body
over time as less and less muscle will be used. Different types of muscle damage symptoms that
MD can cause are muscle degeneration, progressive weakness, fibers splitting, replacement of
muscle tissue with fat and fibrous tissue and fiber death. Some of the most severe cases of MD
can lead to heart failure or loss of breathing ability due to the failure of the corresponding
muscles (NINDS, 2024).
MD is a worldwide genetic disease with multiple forms. The spontaneous gene mutation
can be generational and can come from a family history of the disease. According to NINDS,
MD can be inherited in three ways: “Autosomal dominant inheritance occurs when a child
receives a "normal" gene from one parent and a defective gene from the other parent. Autosomal
recessive inheritance means that both parents carry and pass on the faulty gene. X-linked (or
sex-linked) recessive inheritance occurs when the female parent carrying the affected gene
passes it to the male child.” (NINDS, 2024).
Many of the forms of MD can even have subtypes that categorize the location or effect
that it can have. For example, limb-girdle muscular dystrophy (LGMD), a type of MD that
causes affect to the most proximal muscle involving pelvic and shoulder girdle. This single form
of MD has two primary umbrellas of subtype (Type 1 and Type 2). Beneath these however there
are a complexity of dominant and recessive autosomal subtypes that continue to be discovered.
According to Dr. John D. England in an article about LGMD diagnosis, the complexity of the
genetic disease is staggering, even most neuromuscular experts find it difficult to keep current in
the field (Dr. John D. England, 2014).
Onset and symptoms of MD are variable based on the type and inherited conditions. For
most including LGMD, the onset will be dependent on if the inherited gene type is dominant or
recessive. If recessive this can mean a more rapid onset usually beginning in childhood or late
teen development. In some cases the way MD works can be compounding, therefore the earlier
symptoms appear the more rapid the rate of progression can occur. With MD some forms can be
rapid and cause severe muscle damage early on while other forms can be very slow and cause
very minimal disability.
How can you treat MD?
Treatment for MD does not cure the disease, but it helps people maintain muscle strength,
delay complications, and stay independent longer (Mayo Clinic, 2025). Care usually involves a
long-term, multidisciplinary team. Neurologists, physical and occupational therapists are central
to treatment, while cardiologists, pulmonologists, and other specialists are added depending on
symptoms (Mayo Clinic, 2025).
Management often includes a combination of medications, therapy, and assistive
equipment. Corticosteroids can slow muscle weakening in several types of MD, while newer
gene-targeted medications are available for certain forms of MD (Mayo Clinic, 2025). Physical
and occupational therapy help maintain joint mobility, reduce contractures, and support daily
function. Low-impact aerobic movement, such as walking or swimming, is also encouraged to
promote general health, as long as it is medically approved (Mayo Clinic, 2025).
Assistive devices, including braces, walkers, and wheelchairs and electric chairs help
preserve mobility as muscles weaken. Breathing support may be needed as respiratory muscles
decline, ranging from breathing exercises to nighttime ventilation or mechanical assistance
(Mayo Clinic, 2025). In some cases, surgery is used to correct contractures, address spinal
curvature, or improve heart and lung function (Mayo Clinic, 2025).
Living with MD
Jane was diagnosed with Limb-Girdle Muscular Dystrophy around age ten after early
signs such as toe walking, frequent falls, and some clumsiness. These symptoms prompted a
referral to a neurologist. A muscle biopsy confirmed the diagnosis, and later genetic testing
identified it as Type 2B, a form that does not affect the heart. They learned extensively about the
genetic nature of MD, including the requirement of inheriting the gene from both parents.
Over the years, the understanding of MD has evolved, even though the condition itself has
remained progressive. Jane emphasized that gene-based testing today provides clearer insights
than the muscle-focused testing available during her childhood (Interview, 2025).
Jane relies on tools like a BiPAP machine for nighttime breathing support, a lung
inflation valve bag to assist with limited lung expansion, and a customizable electric wheelchair
that supports driving, transfers, and overall comfort. Jane stays active with physiotherapy and
exercise, which they consider essential to slowing the progression of muscle loss and prolonging
life.
Challenges include difficulty regulating body temperature due to reduced muscle mass,
low circulation, and the natural aging process, which significantly affects recovery. Social
isolation, driving limitations, and are major obstacles. Losing the ability to walk was a
significant emotional and social adjustment. Jane noted that living with MD is extremely
fatiguing, and many people mistakenly confuse it with more well-known conditions like MS
(Interview, 2025).
Motivation comes from determination, consistency with stretching and exercise, and the
belief that maintaining strength slows progression. Jane shared that once muscle function is lost,
it cannot be regained, making it crucial to preserve what remains. Staying positive is not optional
for Jane as she feels she must make the best of what she has (Interview, 2025).
Socially, working and staying active played a major role in maintaining independence and mental
well being. Jane has had to spend a life-time self advocating in order to get what she needs as the
world has slowly adapted to accommodating people with physical disabilities.
For societal changes, Jane hopes to see improved accessibility and better education
around disability, noting that many “accessible” spaces are not truly practical. Technologies and
tools that support independence have been especially valuable.
Jane left me with some advice for someone newly diagnosed, to focus on perseverance,
self advocacy, and refusing to accept limitations placed on them. Jane encourages asking
questions, staying strong, continuing to live fully, and not fearing life or withdrawing from it
(Interview, 2025).
Conclusion
Throughout this blog post, the goal was to highlight what MD is, how it develops, how it
impacts the body, and how treatment focuses on maintaining strength, slowing progression, and
supporting independence. Jane’s experiences offered a real and personal perspective on living
with MD.
For future practicum students and kinesiology professionals, there are several key lessons
to take forward. MD cannot be cured, so treatment is centered around preservation, preserving
mobility, preserving respiratory and cardiac function, and preserving quality of life. This means
exercise must be safe, low impact, and closely monitored, with a strong emphasis on flexibility,
joint health, and maintaining the muscle function that remains.
MD care should be treated as interdisciplinary. Kinesiologists should collaborate with
physiotherapists, occupational therapists, neurologists, and respiratory specialists to ensure a
coordinated approach. Understanding the limits of your scope and working effectively as part of
a broader care team is essential. Empathy and communication are just as important as clinical
knowledge and are a part of the practice. Patients dealing with MD can face fatigue, social
barriers, accessibility challenges, and emotional strain. Building trust, being patient, and creating
an encouraging environment can make a significant difference.
Working with individuals who have MD requires awareness, adaptability, and respect for
the progression of the condition. The more future kinesiologists learn from patient experiences,
the better prepared they will be to support independence, promote function, and contribute
meaningfully to long term management.
References:
Mayo Foundation for Medical Education and Research. (n.d.). Muscular dystrophy and
Treatment. Mayo Clinic.
https://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/diagnosis-tre
atment/drc-20375394
N/A. (2024, December 19). Muscular dystrophy | National Institute of Neurological
Disorders and stroke. Muscular Dystrophy.
https://www.ninds.nih.gov/health-information/disorders/muscular-dystrophy


Tel. (778)-989-5147
betterbodybalance.ca@gmail.com